The brain-body connection and the science behind insatiable hunger
Did you know hunger isn’t just triggered by your stomach? It also involves your brain.
There are specific parts of your brain that control hunger by sending signals to your body, telling it when to eat and when to stop.
One of these areas is called the melanocortin-4 receptor, or MC4R, pathway. Think of it like a road carrying news and information to and from the brain. When this pathway works the way it should, the brain receives a message that it’s satisfied and it’s time to stop eating.
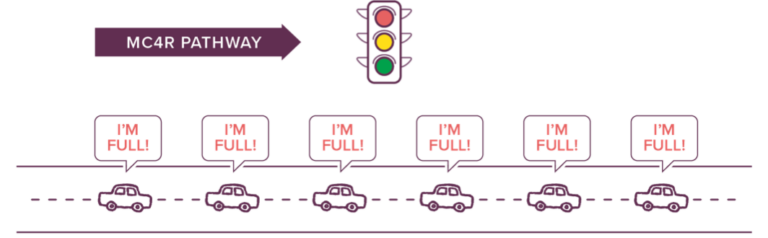
When the traffic light is working, the road is open, and the cars can deliver messages to the brain that the body is full.
In rare genetic diseases of obesity, part of this pathway is broken, so the message can’t be delivered properly, and hunger gets stuck in the “on” position.
The body then believes that it is starving, even though the body has had enough food.
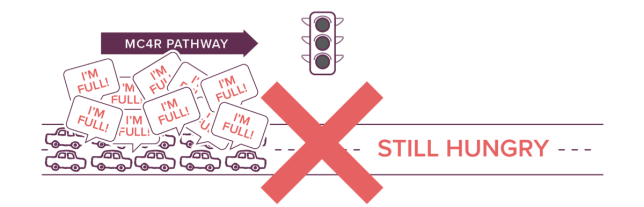
When the traffic light is broken, it causes a traffic jam. Because of this, the cars can no longer deliver messages to the brain that the body is full. Instead, the body believes that it is still hungry.
Watch the videos below for more information
How does hunger work?
How does hunger work in our bodies? Let’s take a closer look.
To understand the science behind it, let’s take a look at what hunger looks like in all of our bodies.
Simply put, we need energy to live. Our bodies need fuel in order to go about our daily lives, in order to perform the functions it needs to stay alive, and we get this energy, we get this fuel, from food.
So our body has many systems in place to make sure that we consume the right amount of food, the right amount of energy to go about and live our daily lives. And when this system is functioning properly, when we are eating as much energy as we are using it to live our lives, this system is in balance and our body weight stays stable, it stays in balance.
When we eat too much food, when we eat more food than our body actually uses in its daily lives, our bodies end up storing this energy as fat tissue, and this is when weight gain occurs.
Now the opposite is also true, if we eat too little food, if we don’t eat enough energy, we don’t have the fuel our body needs to go about and live our daily lives.
Our bodies have natural checks and balances to make sure this balance stays even. We have triggers in our body that tell us when to start eating and when to stop, and hormones act as the messengers.
For more videos like this, don’t forget to check back on our Facebook page and at LEADforRareObesity.com.
Rhythm, LEAD for Rare Obesity, and their logos are trademarks of Rhythm Pharmaceuticals, Inc.
© 2020 Rhythm Pharmaceuticals, Inc. All rights reserved. MC4R-C0281(E)-04.2020
How hunger works in our bodies
Our bodies need energy to function, and we get this energy from food. When functioning properly, the body has systems that balance the food you take in with the energy you need. These natural checks and balances tell us when to eat and when to stop.
The brain-body connection
Our bodies have several processes to balance the food we take in throughout the day with the energy we need to function.
When your stomach is empty, a signal is sent to your brain. Your brain then releases a protein to kickstart your appetite.
Once your stomach is full, a different message is sent to your brain. Your brain then dials down the protein to decrease your appetite and turns up one that is an appetite suppressant.
How do our bodies stay balanced?
Now let’s take a closer look at what we can call the “I’m hungry” cycle.
Now, imagine an empty stomach with no food in it. Basically, representing a body that is low on energy and needs fuel. When this happens, hormones from the body report this low status to the brain, sending the message of, “I’m empty, eat something.” The brain gets this message and in turn, releases a protein to stimulate the appetite.
The opposite also occurs when we have the “I’m full” cycle. Once there is food in the stomach, representing a body that has enough energy, a message is sent to the brain telling it, “I’m full, stop eating.” The brain then goes ahead and dials down that protein that stimulated the appetite and cranks up the one that is an appetite suppressant so that the person stops eating.
For more videos like this, don’t forget to check back on our Facebook page and at LEADforRareObesity.com.
Rhythm, LEAD for Rare Obesity, and their logos are trademarks of Rhythm Pharmaceuticals, Inc.
© 2020 Rhythm Pharmaceuticals, Inc. All rights reserved. MC4R-C0281(F)-04.2020
The brain’s hunger pathways
So, how do our brains make sense of all these messages telling it to eat something, or stop eating?
How does it know when to send those appetite stimulating, or suppressing signals?
The specific part of our brain that accepts these messages, and makes sense of them, is called the hypothalamus. Think of the hypothalamus as a neighborhood within the brain. In this neighborhood, there is a road called the MC4R pathway.
On this road, cars travel carrying news and information, to and from the brain. These cars on the MC4R pathway are proteins and hormones that communicate with each other to control hunger, and regulate our energy balance.
In individuals with a rare genetic disorder of obesity, this process does not work as it should. A genetic variant, or a change in the body’s DNA, causes part of this pathway to not work properly.
Think of one of the roads as blocked, and the cars can’t get through. When this happens, the signals in the hypothalamus get stuck in the “I’m hungry” cycle, because the “I’m full” message cannot get through and be delivered. The brain doesn’t get this message and believes that the body is starving, even though there is food in the stomach. Without this message or signal, this can cause insatiable hunger and ultimately lead to extreme weight gain early in life.
For more videos like this, don’t forget to check back on our Facebook page and at LEADforRareObesity.com.
Rhythm, LEAD for Rare Obesity, and their logos are trademarks of Rhythm Pharmaceuticals, Inc.
© 2020 Rhythm Pharmaceuticals, Inc. All rights reserved. MC4R-C0281(C)-01.2020
Making sense of the signals
There are many parts in the brain that communicate with each other to regulate hunger. One of these areas is called the MC4R pathway. Think of it like a road carrying news and information to and from the brain.
When this pathway works the way it should, the brain receives a message that it’s time to stop eating. In rare genetic diseases of obesity, part of this pathway is broken, and the body and brain can’t communicate to each other properly. The brain doesn’t get the message when the stomach is full and believes that the body is starving, even though the body has had enough food.